In Vitro Fertilization
7305041486
Introduction
Many couples faced with infertility are still unable to become pregnant after first line therapy such as ovulation induction, intrauterine insemination, or reproductive surgery. For these couples, the logical next step is to explore the Assisted Reproductive Technologies (ART).
In vitro fertilisation is a demanding procedure with emotional, physical and financial consequences. Couples are often only considered for IVF, if surgery, drug therapy and IUI have not been successful. Previously, only couples whose fertility problem was the result of blocked fallopian tubes were considered for IVF. However today, its use has extended to include couples affected by endometriosis, severe male infertility and long-term unexplained infertility.
It is important not to underestimate the demands of IVF. However as long as you prepare yourselves properly as a couple and talk about it openly and honestly, the chances are greater that you will come through the treatment well, irrespective of the outcome. The information in this section provides greater insight into the world of IVF. In this way, you will arm yourself with knowledge, which you can use to find your way in this difficult, but possibly worthwhile process.
Most IVF clinics have extensive information about IVF treatment. Make sure you read this as details of the treatment can vary from clinic to clinic. Once you have been selected for IVF treatment, it is important to find out as much as you can about the way IVF is performed at your clinic. As soon as it becomes apparent that IVF is appropriate for your situation, you can be placed on the waiting list for treatment. This waiting list can vary greatly from clinic to clinic. However, it is generally preferable to undergo treatment at the fertility clinic you are already attending due to the relationship that you have built up with the people treating you to date, or, if not available there, locally because of the travelling time associated with the frequent checkups.
The IVF Process
IVF treatment is made up of the following key phases
Stimulation of the ovaries: As several egg cells are required for IVF to maximize the chances of fertilization, the ovaries are stimulated with drug therapy.
The outcome
2 weeks later you will find out whether treatment has succeeded.
Preparation :
As soon as you are put on the waiting list for IVF an extensive consultation will take place. This will include a verbal explanation of the procedure (supported by written information) where obviously you will have the opportunity to ask questions. It is critical that everything is clear to both partners before beginning treatment. You will also be told how to use the various drug therapies needed and, where appropriate, you will be taught how to administer them. The preliminary examinations that have to take place will also be discussed with you. These might include, for example, an extra blood test (for infectious diseases or hormone assessment), or another semen analysis. Additional heredity tests (chromosomal studies) on a blood sample from the man in the case of ICSI treatment. You will also be given further information on daily practice in your clinic; it is essential that you know whom to contact, and when, if you have questions or problems. IVF treatment not only takes up a lot of time, but also demands considerable flexibility. The course and duration of the stimulation is not easy to predict, as a result of which follow-up checks and even the day of the puncture to collect the eggs can only be scheduled shortly in advance. It is important that you bear this in mind during the month of your treatment.
Treatment Plan :
There are different types and brands of the drugs that may be prescribed to you. The precise drug therapies you use will depend on your personal situation and the clinic’s general policy. Usually the women’s own hormone production must be suppressed initially. Various methods are available for this.The woman then begins daily injections to stimulate the ovaries to produce a number of egg cells. Ideally the aim is to obtain 10 (5 – 15) egg cells. The quantity of drugs (dosage) required for this is estimated in advance. Do not expect from the start, however, to always be able to predict how the ovaries will react. If there are too many egg cells, your treatment may have to be cancelled. If the reaction is moderate, the dosage can sometimes be increased during the treatment, but a treatment may also be cancelled if there are too few egg cells. Although disappointing, you can at least take some solace from the fact that this experience can be used to improve the chance of success for a possible subsequent IVF treatment.
Checkups :
The egg cells are found in fluid-filled follicles in the ovaries. The size of a follicle provides an indication of the maturity of the egg cell. During the treatment, you will have frequent checkups at the outpatients department to track the reaction of the ovaries to drug therapy using vaginal ultrasonography. The size of the follicles and the viscosity (thickness) of the cervical mucus are measured at each check-up to determine the right time for the puncture. Blood may also be taken to measure the hormone levels.
Puncture :
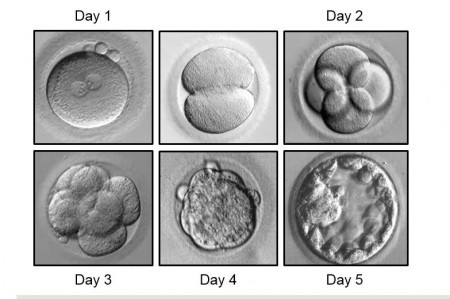
Fertilisation :
Embryo Transfer :
Frozen Embryos (Cryopreservation) :
Suitable candidates for IVF are
Tube pathology
If both fallopian tubes are completely blocked, IVF is directly indicated. If the function of the fallopian tubes is reduced, IVF is only considered after other treatments. Endometriosis Depending on the severity, drug or surgical treatment will be the indicated treatment in the first instance. IVF is considered if a pregnancy has not occurred after treatment. For mild forms of endometriosis, the guidelines for unexplained subfertility are applied.
Male subfertility
ICSI is also considered in severe cases of subfertility. In less severe forms, IVF is considered after a number of IUI cycles.
Premature ovarian failure
Unexplained subfertility
No cause found after full investigation, at least 3 years of marriage, and having completed alternative approaches to fertility management for at least 1 year. However, this will not apply to female above 35 years old. Other conditions acceptable to the local obstetric/gynaecologic community. IVF shall only be carried out on a married woman and only with the consent of her husband, whether or not her husband’s semen is used. The most important reason for considering a couple for IVF at an earlier stage is the age of the woman: the chances of a pregnancy over the age of 35 rapidly reduce, and with them the chances of success after IVF. The doctor treating you will assess when and if IVF is an option for you. A strict selection is justified given that IVF is an invasive and intensive treatment with associated risks.
When does IVF not make sense?
Age
The success rate of an IVF treatment reduces with age. As the age of the woman increases, there is a greater chance that the ovaries will no longer react fully to the stimulation. This can be assessed from certain blood results, including the FSH level. In addition, the quality of the egg cells reduces and the risk of miscarriage is greater as age increases. This is therefore the reason why women over the age of 40 are generally no longer considered for IVF treatment.
Sperm Quality
Limitations caused by conditions relating to sperm quality have been enormously relaxed by the introduction of ICSI.
Risks
Weight
Being seriously overweight not only has an effect on fertility, but also on general health and therefore on a possible pregnancy. In addition, ovaries for IVF have to be accessible for puncture. Sometimes this is scarcely possible in heavier women. Therefore, weight loss is a necessity in some cases before a possible treatment.
Pregnancy
The woman has to be able to carry a pregnancy to term.
The IVF clinic concerned will carefully map out your situation, after which it will decide whether you can be considered for IVF.
Success Rates
How great are the chances of success?
In an IVF treatment, the chance of pregnancy per cycle is around 20% on average. However, this is highly dependent on individual circumstances such as age, sperm quality and the number and quality of the embryos. In addition, not all pregnancies lead to a live-born child. 1/4 of all pregnancies begun end in a miscarriage (20% of the total) or in an ectopic pregnancy (5%).
Because there are new chances with every cycle, half the couples on average return home with one child or more after three attempts.IVF results can be displayed in various ways. The following definitions have been used:
Started cycle
IVF attempt, from the start of the drugs to stimulate follicle growth.
Follicle puncture
Ovary puncture with the aim of obtaining egg cells.
Embryo Transfer
Placing of embryos in the uterine cavity.
Pregnancy
Positive test in urine or serum (>50 IE/L), no earlier than 15 days after the puncture.
On-going pregnancy
Intact intra-uterine pregnancy, > 10 weeks after the puncture.
Confidence interval
Interval in which there is a 95% certainty.
The number of continuing pregnancies per cycle started has been chosen as the method of recording and comparing the IVF figures. This percentage tells us something about the care delivered by a centre – but is far from the whole story.
Firstly, this percentage is dependent on all sorts of other factors, such as the age of the woman, the length of time she has wanted a child and the number of previous treatments. These factors may vary from centre to centre. For example, if a centre primarily treats older women, that centre’s chances of a pregnancy will be lower.
Secondly, this percentage may vary from year to year for unpredictable causes. It therefore makes sense to look at the results over several years.Finally, other factors such as patient satisfaction, the percentage of complications and the percentage of multiple births are also important to the quality of care. If several embryos are transferred, for example, not only do the chances of a pregnancy increase, but so also do the chances of multiple births with all the associated risks.