Infertility Diagnosis
7305041486
Introduction
The purpose of this proposal is to outline suggested clinical pathways for the management of infertility and common reproductive endocrinology problems. The goal is to create an approach that provides the greatest success while using limited resources in the most cost-effective fashion.
A traditional approach to the management of Reproductive Endocrinology & Infertility problems can be found in any traditional text. However, most texts do not take into account the limited availability of resources within a managed care environment, and do not address the issue of stratification of care into that provided by an OB/GYN generalist and that provided by the reproductive endocrinology subspecialist.
To that end, this outline will attempt to focus on what care is best provided by which practitioner. To design a cost-effective, medically appropriate evaluation and treatment plan, we must take the patient’s age into consideration. While there is little necessity to initiate aggressive therapy for the 20 year old with unexplained infertility, those over 35 deserve a more aggressive approach.
Initial Infertility Evaluation Complete history and physical examination
Obtain all previous medical records for treatment related to infertility, hormonal or menstrual disturbances, anovulation, gynecologic surgery, or pelvic infection. Appropriate medical information should be gathered on the husband. Particular attention needs to be directed toward a review of medications that may interfere with fertility (i.e. Calcium channel blockers or atorvastation in males) or those that might be teratogenic.
Initial Medical Laboratory Evaluation
TSH, Prolactin, CF screen, CBC, ABO, RH-Type and antibody screen, HIV, HBsag, HCab, VDRL, Chlamydia/GC DNA probe, PAP smear, midluteal am progesterone above 10 ng/ml suggests normal ovulation. (Progesterone levels may drop up to 50% by the afternoon and after a meal.)
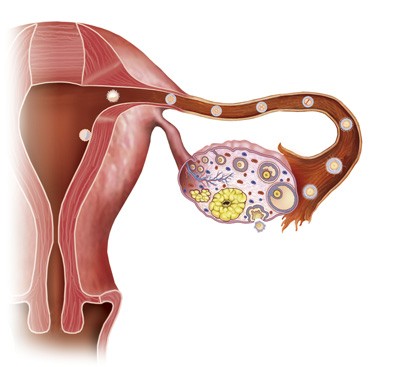
Evaluation of Ovulation
BBT charts from up to 3 months may be reviewed. While patients may be encouraged to initially record BBTs, these charts are only of value retrospectively determining that the patient has in fact ovulated and are of little value predicting when ovulation will occur
Individualized Laboratory Testing
African American: Sickle screen and thalasmeia as appropriate.
Over 30
FSH and estradiol may be obtained on cycle day 3 along with an antral follicle count ultr. Antimullerian Hormone, AMH testing can be done on any cycle day. FSH values above 10 miu/ml or AMH <0.4 should result in REI review. Ultrasound screening for ovarian volume and antral follicle count on cycle day 3 may enhance the sensitivity of ovarian reserve monitoring
Irregular Menses
Irregular Menses with Hirsutism, Acne or Obesity
The free testosterone panel may be helpful to monitor the effectiveness of metformin therapy. Fasting am 17 hydroxyprogesterone is ordered during the follicular phase if adult onset congenital adrenal hyperplasia is suspected. Values above 150 deserve referral for cortrysyn stimulation testing. If the patient appears Cushingoid, decadron 1mg is administered at midnight and an 8am fasting cortisol level is obtained the next morning. If PCOS is suspected, cardio C-reactive protein, homocysteine and a lipid panel should be ordered.
Low risk for tubal disease
Semen Analysis
For those with azoospermia, FSH, free testosterone panel, estradiol, chromosomal analysis and Y microdeletion tests are indicated.
Tubal Factor Infertility
Assessment of Risk Factors:
Dyspareunia
Dysmenorrhea, if associated with pelvic tenderness, uterosacral nodularity or perimenstrual diarrhea, should be considered evidence of endometriosis.
Evaluation of Tubal Factors
- Over 35, > 3 years infertility & risk factors: Tubal patency should be determined preoperatively to rule-out proximal tubal obstruction that can be treated during an initial laparoscopic procedure. Laparoscopy or IVF should be considered early in the evaluation.
- Low risk factors, anovulatory infertility or AID candidates: HSG may be delayed if no risk factors are present. Ovulation induction or AID (donor insemination) may be considered for 3-4 cycles before considering HSG. A recent study has shown that one additional pregnancy will occur for every 60 diagnostic laparoscopies performed in women with low risk of tubal disease resulting in a cost of~$600,000 per additional pregnancy. IVF is far more cost effective than diagnostic laparoscopy in women without significant risk factors.
Post-coital Testing has not been shown to correlate well with fertility and therefore is rarely indicated.
Endometrial Biopsy: The routine use of endometrial biopsy to confirm the adequacy of luteal phase has poor predictive value for the management of infertility. It is only indicated for those patients with regular cycles and recurrent pregnancy loss. Endometrial biopsy, therefore, is not indicated in the diagnosis of infertility.

