Preimplantation Genetic Diagnosis
7305041486
Introduction
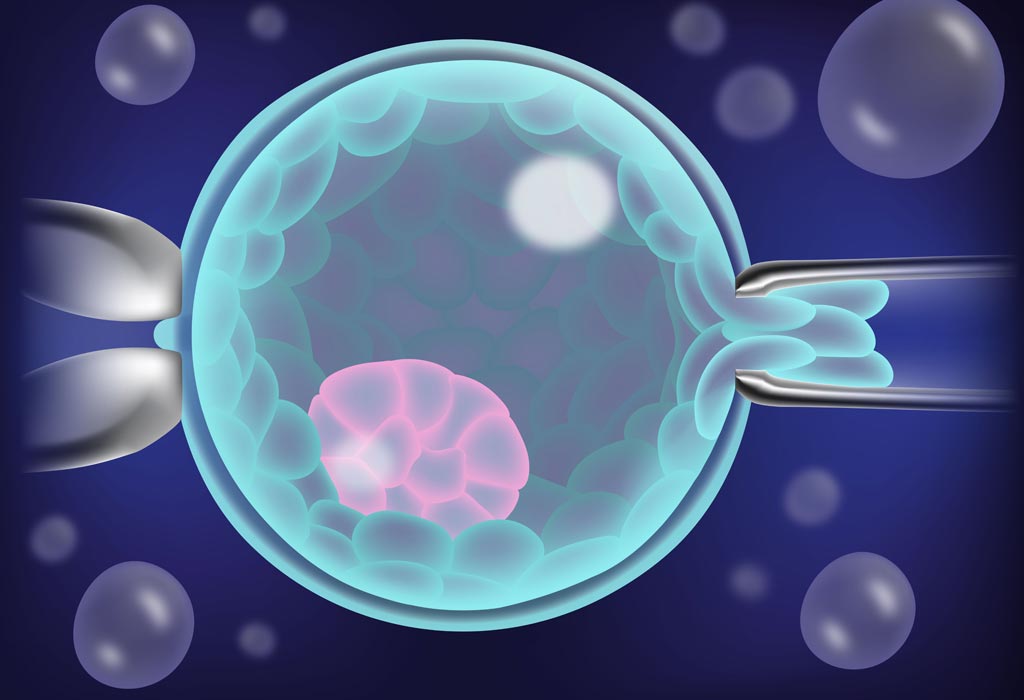
Preimplantation genetic testing is a technique used to identify genetic defects in embryos created through in vitro fertilization (IVF) before pregnancy. Preimplantation genetic diagnosis (PGD) refers specifically to when one or both genetic parents has a known genetic abnormality and testing is performed on an embryo to determine if it also carries a genetic abnormality. In contrast, preimplantation genetic screening (PGS) refers to techniques where embryos from presumed chromosomally normal genetic parents are screened for aneuploidy. Because only unaffected embryos are transferred to the uterus for implantation, preimplantation genetic testing provides an alternative to current postconception diagnostic procedures (ie, amniocentesis or chorionic villus sampling), which are frequently followed by the difficult decision of pregnancy termination if results are unfavorable. PGD and PGS are presently the only options available for avoiding a high risk of having a child affected with a genetic disease prior to implantation. It is an attractive means of preventing heritable genetic disease, thereby eliminating the dilemma of pregnancy termination following unfavorable prenatal diagnosis
Indications for Preimplantation Genetic Diagnosis
Preimplantation genetic diagnosis (PGD) is recommended when couples are at risk of transmitting a known genetic abnormality to their children. Only healthy and normal embryos are transferred into the mother’s uterus, thus diminishing the risk of inheriting a genetic abnormality and late pregnancy termination (after positive prenatal diagnosis).
Primary candidates for PGD, These include the following
Couples with a family history of X-linked disorders (Couples with a family history of X-linked disease have a 25% risk of having an affected embryo [half of male embryos].)
Couples with chromosome translocations, which can cause implantation failure, recurrent pregnancy loss, or mental or physical problems in offspring
Carriers of autosomal recessive diseases (For carriers of autosomal recessive diseases, the risk an embryo may be affected is 25%.)
Carriers of autosomal dominant diseases (For carriers of autosomal dominant disease, the risk an embryo may be affected is 50%.)
Conditions diagnosed using PGD
Sex-Linked Disorder
Single gene defects
Chromosomal Disorders
Sex-Linked Disorder
X-linked diseases are passed to the child through a mother who is a carrier. They are passed by an abnormal X chromosome and manifest in sons, who do not inherit the normal X chromosome from the father. Because the X chromosome is transmitted to offspring/embryos through the mother, affected fathers have sons who are not affected, but their daughters have a 50% risk of being carriers if the mother is healthy. Sex-linked recessive disorders include hemophilia, fragile X syndrome, most neuromuscular dystrophies (currently, >900 neuromuscular dystrophies are known), and hundreds of other diseases. Sex-linked dominant disorders include Rett syndrome, incontinentia pigmenti, pseudohyperparathyroidism, and vitamin D–resistant rickets.
Single gene defects
PGD is used to identify single gene defects such as cystic fibrosis, Tay-Sachs disease, sickle cell anemia, and Huntington disease. In such diseases, the abnormality is detectable with molecular techniques using polymerase chain reaction (PCR) amplification of DNA from a single cell. Although progress has been made, some single gene defects, such as cystic fibrosis, have multiple known mutations. In cystic fibrosis, only 25 mutations are currently routinely tested. Because most of these rare mutations are not routinely tested, a parent without any clinical manifestations of cystic fibrosis could still be a carrier. This allows the possibility for a parent carrying a rare mutation gene to be tested as negative but still have the ability to pass on the mutant cystic fibrosis gene.PGD can also be used to identify genetic mutations like BRCA -1, which does not cause a specific disease but increases the risk of a set of diseases.
Chromosomal Disorders
The last group includes chromosomal disorders in which a variety of chromosomal rearrangements, including translocations, inversions, and deletions, can be detected using fluorescent in situ hybridization (FISH). FISH uses telomeric probes specific to the loci site of interest. Some parents may have never achieved a viable pregnancy without using PGD because previous conceptions resulted in chromosomally unbalanced embryos and were spontaneously miscarried.
Indications for Preimplantation Genetic Screening
Most early pregnancy losses can be attributed to aneuploidy. Because only chromosomally normal embryos are transferred into the uterus, the risk of first and second trimester loss is markedly reduced. At present, no specific list of indications for preimplantation genetic screening (PGS) is available.
Primary candidates for PGS can include the following
Women of advanced maternal age
Couples with history of recurrent pregnancy loss
Couples with repeated IVF failure
Male partner with severe male factor infertility
These patient populations are at risk of failure with IVF because of a high proportion of aneuploid embryos. PGD is believed to decrease this risk by selecting chromosomally normal embryos that have a higher chance of implantation.Advanced Maternal Age:
The risk of aneuploidy in children increases as women age. The chromosomes in the egg are less likely to divide properly, leading to an extra or missing chromosome in the embryo (see Table 1). The rate of aneuploidy in embryos is greater than 20% in mothers aged 35-39 years and is nearly 40% in mothers aged 40 years or older. The rate of aneuploidy in children is 0.6-1.4% in mothers aged 35-39 years and is 1.6-10% in mothers older than 40 years. The difference in percentages between affected embryos and live births is due to the fact that an embryo with aneuploidy is less likely to be carried to term and will most likely be miscarried, some even before pregnancy is suspected or confirmed. Therefore, using PGD to determine the chromosomal constitution of embryos increases the chance of a healthy pregnancy and reduces the number of pregnancy losses and affected offspring.One of the most frequent aneuploidies, trisomy (ie, 3 identical chromosomes present in the embryo), is trisomy of chromosome 21, which leads to Down syndrome. This particular abnormality also frequently leads to spontaneous miscarriage, the precise frequency of which is difficult to determine. Thus, the only reliable information is on the frequency of babies born with Down syndrome. An informative article in the Journal of the American Medical Association [4] includes information on estimating the incidence of trisomy 21/Down syndrome in fetuses at 16 weeks of pregnancy (also see Table 2). Recurrent pregnancy loss (RPL) is usually defined as 2 or more consecutive pregnancy losses before 20 weeks’ gestation. The cause is frequently unknown but may be secondary to fetal anomalies or uterine abnormalities. Chromosomal abnormalities are noted in 50-80% of abortuses,[8] and couples with RPL have a higher percentage of aneuploid embryos than patients without RPL.[9] However, the use of PGS does not improve the pregnancy rate in this group of patients but increases the likelihood of delivery at term.[10] PGS also benefits the subgroup of patients who have proven abnormal concepti by cytogenetic analysis.
Recurrent IVF Failure
Recurrent IVF failure (RIF) is usually defined as 3 or more failed IVF attempts involving high-quality embryos. Evidence suggests that this patient population has a higher number of chromosomally abnormal embryos.[11] However, no study has shown an improvement in pregnancy rate with PGS in patients who have a history of RIF. Although most IVF failures can be accounted for by embryonic aneuploidy, various immunological and uterine factors likely contribute to implantation failure.
Male factor infertility
Gonadal failure in men has been linked to the generation of embryos with an increased incidence of inherited and de novo chromosomal abnormalities. Normal fertile men have approximately 3-8% of sperm that are chromosomally abnormal. This risk increases significantly in men with severe infertility (ie, low sperm count, poor morphology, and poor motility) to approximately 27-74% abnormal spermatozoa.[12] With the introduction of intracytoplasmic sperm injection (ICSI) in assisted reproductive techniques, clinicians have given men with poor sperm quality the opportunity to overcome natural selection and successfully produce a zygote.Various genetic defects have been found to be associated with male factor infertility. This includes aneuploidy, most commonly Klinefelter syndrome, Robertsonian translocations, Y chromosome microdeletions, androgen receptor mutations, and other autosomal gene mutations (eg, cystic fibrosis transmembrane conductance regulator gene and sex hormone-binding globulin gene mutations).[13] Therefore, a high risk of transmission of genetic mutations to the patient’s offspring is associated with IVF involving ICSI.
The use of PGS/PGD in couples with severe male factor infertility may decrease pregnancy rates but also limits the prevalence of chromosome abnormalities. Data are insufficient to recommend routine genetic screening of all embryos in this group of patients. However, if couples do choose to proceed with PGS/PGD, they should be properly counseled on the decreased chance of conception due to the likely reduced number of normal embryos available to transfer.